By Prof. David Bowen
Read the whole article and join the conversation in MDSEUROPE, a blog for MDS stakeholders, part of the MDS-RIGHT programme.
I constantly question why, of the many MDS patients who are looked after in hospitals big and small in the UK, so few come to see MDS experts in order to discuss their disease in more detail. Why is this? Do I perceive a problem that does not exist? Maybe most patients simply don’t want any more information? But what if they do?
Barriers to referral
Here are a few obvious possibilities, all of which could be logical:
The patient/relative has enough information already
The patient/relative does not know that they could obtain more information, for example in relation to their specific type of MDS, or clinical trials
The patient/relative would like more information but really likes the doctor looking after them and does not want to upset her/him.
The doctor is too busy to spend time creating a referral or discussing the disease in detail.
The doctor knows enough about MDS and there are so few treatments available that the MDS specialist could not advise better than them. All of their patients are discussed by the local team in the hospital’s multidisciplinary team meeting as specified in the national quality standards.
The healthcare system provides perverse disincentives to referral (typically personal physician financial issues)
Patient organisations are trying hard
In the UK we have one of the most active and effective MDS Patient Support organisations, which is contacted regularly by patients and relatives. So why does this not produce a flood of referrals to specialist hospitals?
Patient Support Groups are very worthy advocates for patients and relatives but can generally only respond to approaches from patients. There are also active local support groups and other outreach initiatives in many regions /countries but the whole system tends to serve the more proactive and internet-literate section of the population, which are enriched by the middle classes and/or those with a strong family support network. A large swathe of the MDS patient population chooses not to access these services or perhaps is not aware of their existence, or exactly what they can offer.
All newly diagnosed MDS patients should be provided with the UK patient information booklet, which includes the following statements:
There are a number of UK centres with a specialist interest in treating patients with MDS; some of which are recognised as Centres of Excellence.
You can request to be referred to these specialists for an additional opinion and a referral request can be made via your GP or your local haematologist. These referrals are particularly helpful for the more complex MDS cases.
Please note that additional opinions are sought by many patients across the UK. These are perfectly reasonable requests, given that MDS is a rare and complex disease. Although all haematologists will be familiar with the condition, not all of them will have the specific expertise found in specialist centres. After you are seen at a specialist centre for your additional opinion, you will still be treated at your local hospital and your local haematologist will work together with the specialist to provide you with optimal care.
A specialist centre will also provide you with a dedicated Clinical Nurse Specialist – whom you will be able to consult between appointments if necessary.
What more can we do? Why should patients see a specialist anyway?
The main reason that I want to see MDS patients is simply to offer them more information about their specific type of MDS in the context of their medical / social background. I do not expect to necessarily change a management plan in many patients, but information is power.
Almost all patients that I see, find the extra information enlightening and helpful. I believe that a one-off specialist consultation should be offered to all newly diagnosed patients who are physically able to travel to a specialist centre. Information is power.
A simple example of this was a patient diagnosed with IPSS INT-1 and given the median survival of 3.5 years. She retired early from work and planned her remaining life for this survival duration although she required no active therapy. She asked for referral to a specialist and we discussed her updated prognosis in the light of IPSS-R, which she was not familiar with. Her IPSS-R category was ‘Very Low’ and median survival predicted to be 8.8 years. Still only requiring active monitoring and 3 years since diagnosis, she completely changed her approach to life. Information is power.
There is an evidence base for reduction of uncertainty as one aspect of ‘value’ in healthcare and although a specialist may be able to achieve this, the heterogeneity of MDS given the current state of knowledge will always be problematic for precise prognostic and predictive discussions.
If I have a clinical trial available I would like all suitable patients who can get to my centre to be offered the opportunity to participate. The UK has a national public website for all cancer trials; does the public know about it? In Leeds we publicise our clinical trials through websites (local and national) and (repeated) direct emails to all regional Haematology consultants – we receive relatively few referrals for trials.
Statement in national guidelines
In a recent revision of the UK BCSH MDS management guidelines I insisted that we retain the following statement that I wrote at the start of the document (despite some objections from some members of the Sounding Board and other informal mutterings of discontent):
As MDS is considered a rare or ‘orphan’ malignancy, patients should always be given the opportunity to be reviewed by a regional or national haematologist with a specific interest in MDS.
Thus far, this has had no impact to my knowledge.
So, who is an MDS ‘expert’?
How can patients distinguish the most expert ‘experts’ working internationally and with a clinical practice with many MDS patients / decades of experience of MDS, from the interested but less experienced ‘expert’ or a local expert that looks after myeloid disorders in their hospital.
I don’t know the answer, but I do know that if a member of my family or I have a serious illness, I will fight hard to see one of the best doctors in the UK for that condition. Why is this not the norm?
European initiatives for patient advocacy specific to MDS
One of the key goals of MDS-RIGHT is improved dissemination of information to all patients and carers/relatives, working with patient support groups. The recently launched EuroBloodNet is another networking initiative with high potential in this area.
Questions for you, commenters…
I would be very interested to understand if this issue is widespread in Europe and if so how should we address this?
Have you identified any strategies to encourage/empower patients to request referral to specialists?
Can we emphasise to patients / local doctors that the fact that not many drugs are approved for MDS does not mean that an expert cannot help an MDS patient with information that is very useful to them? How do we get this message across?
David acknowledges the expert input from Sophie Wintrich, UK MDS Patient Support Group. This is a shortened version of an expanded article that will shortly be posted on the UK MDS Patient Support Group and the MDS Alliance websites.





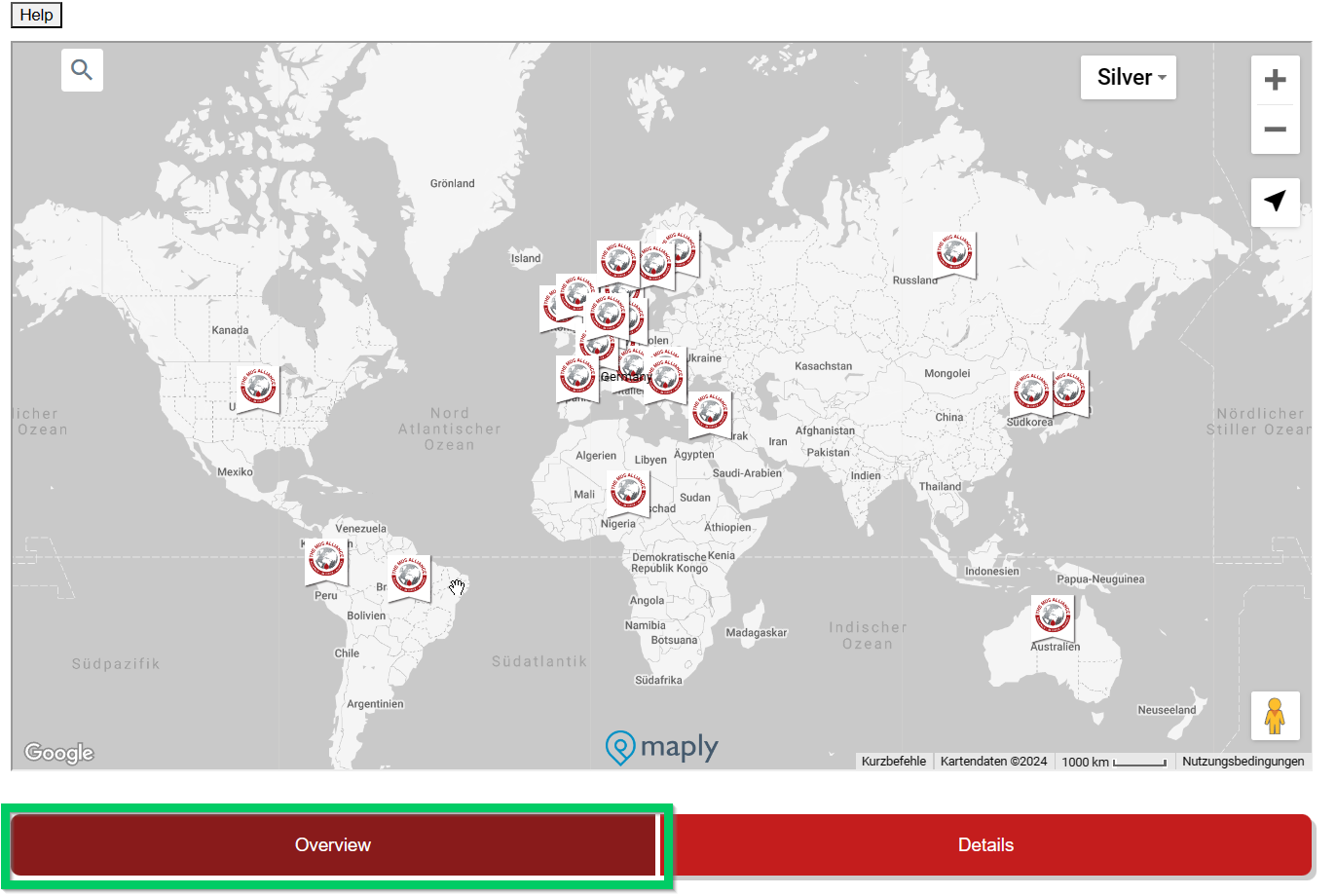

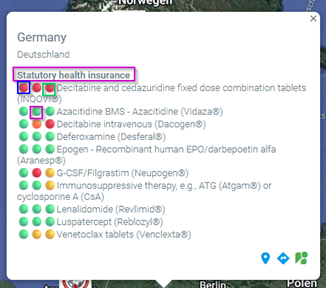 This overview is interactive and detailed information is displayed by moving the mouse. Under the country name there is a (pink) reference to the health insurance system (if known) in this country.
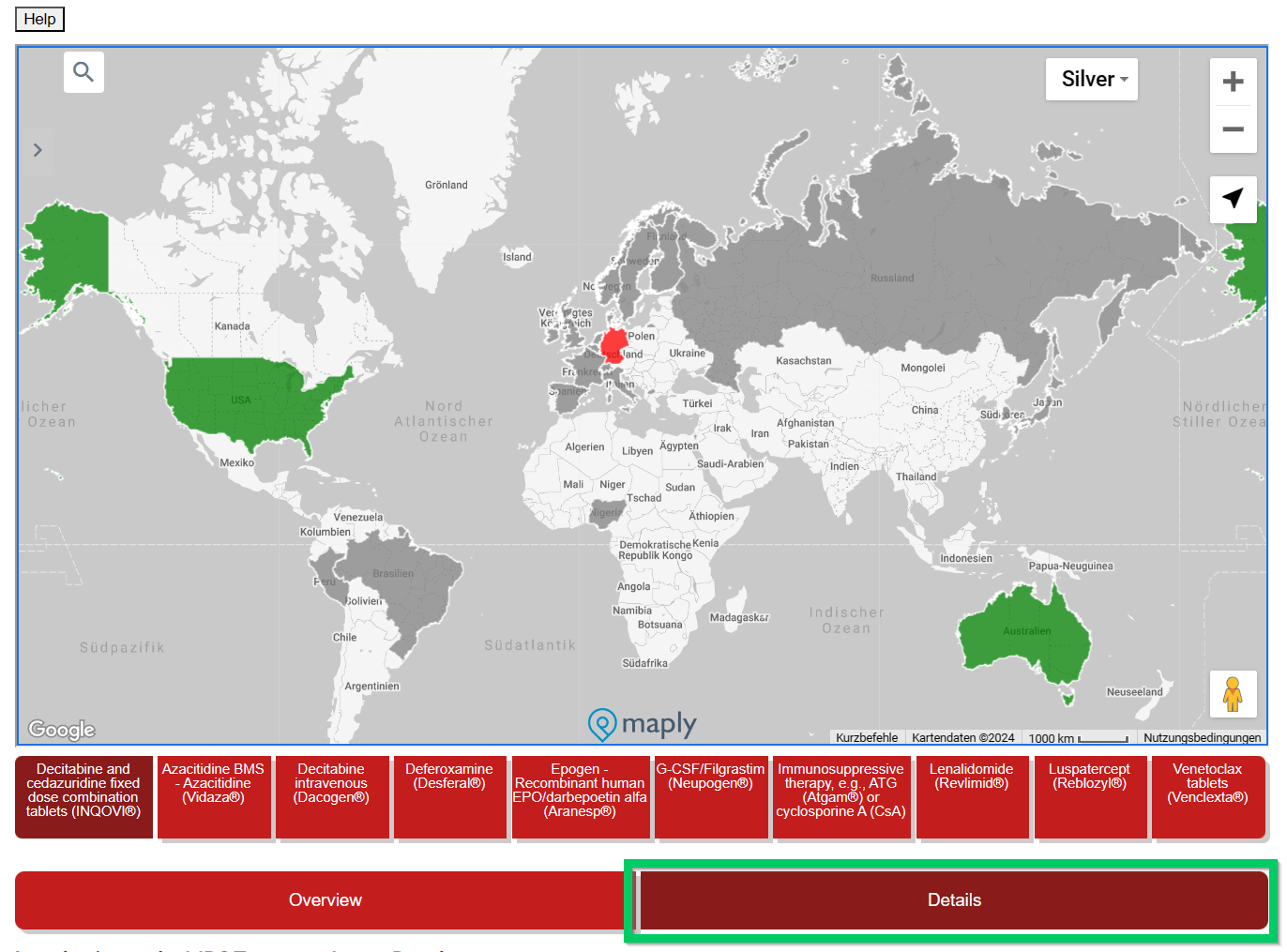
This overview is interactive and detailed information is displayed by moving the mouse. Under the country name there is a (pink) reference to the health insurance system (if known) in this country.



