By Patrick Festy –
Read the whole article and join the conversation in MDSEUROPE, a blog for MDS stakeholders, part of the MDS-RIGHT programme.
What do we mean by fatigue?
When questioned about our disease, we and our doctors speak first of fatigue, but most words that are used — weariness, tiredness, numbness, heavy legs, stiff muscles, short breath — are not strong enough.
One patient describes it aptly:
It’s more a sensation of exhaustion than tiredness. I asked: Why am I like this? Why can’t I do the things I should be doing? I was told: You are tired, that’s normal, you are over 60, you are a grandparent, you want to continue to be active, but it’s normal. No, I felt, it’s not normal. I am not tired, I am totally exhausted. Something is wrong with me.
The widow of an MDS patient said:
Few of those they share their lives with or who assist them can comprehend the harassing fatigue that MDS patients suffer. My husband used to say: “We wonder if the specialists who are caring for us understand what this fatigue is really like.”
But fatigue is not the whole story. For MDS patients it is associated with symptoms that do not necessarily have a clinical link to MDS but are nevertheless an intimate part of patients’ experience and reinforce the repercussions of fatigue on daily living. Efficace (2014) shows notably that loss of appetite, respiratory problems and insomnia accompany severe fatigue among high risk MDS patients.
…
When we studied the effects of fatigue on quality of life of the members of our patients’ group in 2012-2013 we also discovered the effects of symptoms and problems often associated with MDS: loss of appetite, respiratory problems, susceptibility to infections and bleeding. The impact is as much psychological as physical. MDS patients surveyed were 25% less likely than other members of their age group to be able to do “what they were used to doing” and thereby experienced greater physical limitations. But they were also 26% more likely to “fear that their condition would get worse” than others in their age group and thereby experienced greater emotional distress.
…
Self reported fatigue provides prognostic information and should be included in routine diagnostics and controlled trials
Efficace et al. (2014) results confirm:
Patient-reported fatigue severity, rather than the degree of anemia, more accurately revealed the effects of disease burden on the patients’ well-being and daily functioning.
But Efficace (2015) goes one step further:
In patients with newly diagnosed higher-risk myelodysplastic syndromes self-reported fatigue severity provides prognostic information for survival independent from gold-standard risk classifications.
He concludes that fatigue assessment should be included in routine diagnostic investigation for these patients and considered as a standard Baseline stratification factor in future randomised controlled trials.
…
In conclusion, improvement in physicians’ perception of their patients’ health status and preferences for involvement in treatment decisions is necessary.
The importance of considering patients’ quality of life, along with objective quantitative criteria to measure the success of treatments, has long been recognized and efforts to clarify and rationalize these criteria by the IWG 2006 include a few words on the subject, but implementation remains extremely timid.
Quality of Life as a dimension of the success or failure of a treatment
We advocate that all clinical trials integrate patients’ quality of life as a dimension of the success or failure of a new treatment, considered on an equal basis with the concepts of remission, transfusion independence, progression-free survival, etc. For this to be possible researchers will have to reach a consensus on quality of life indicators to be used in trials.





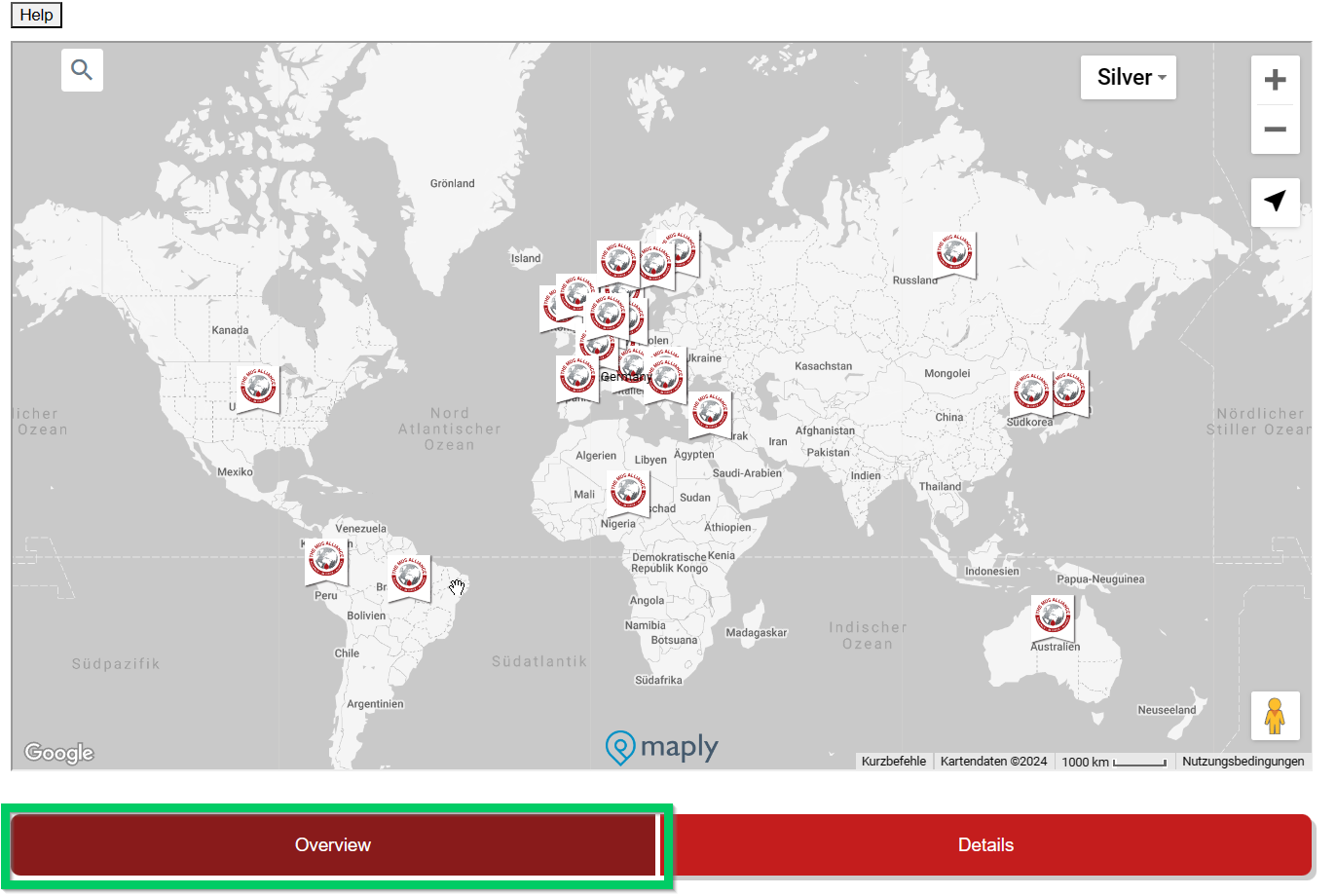

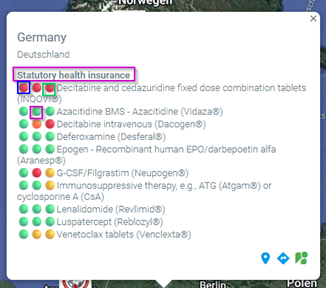 This overview is interactive and detailed information is displayed by moving the mouse. Under the country name there is a (pink) reference to the health insurance system (if known) in this country.
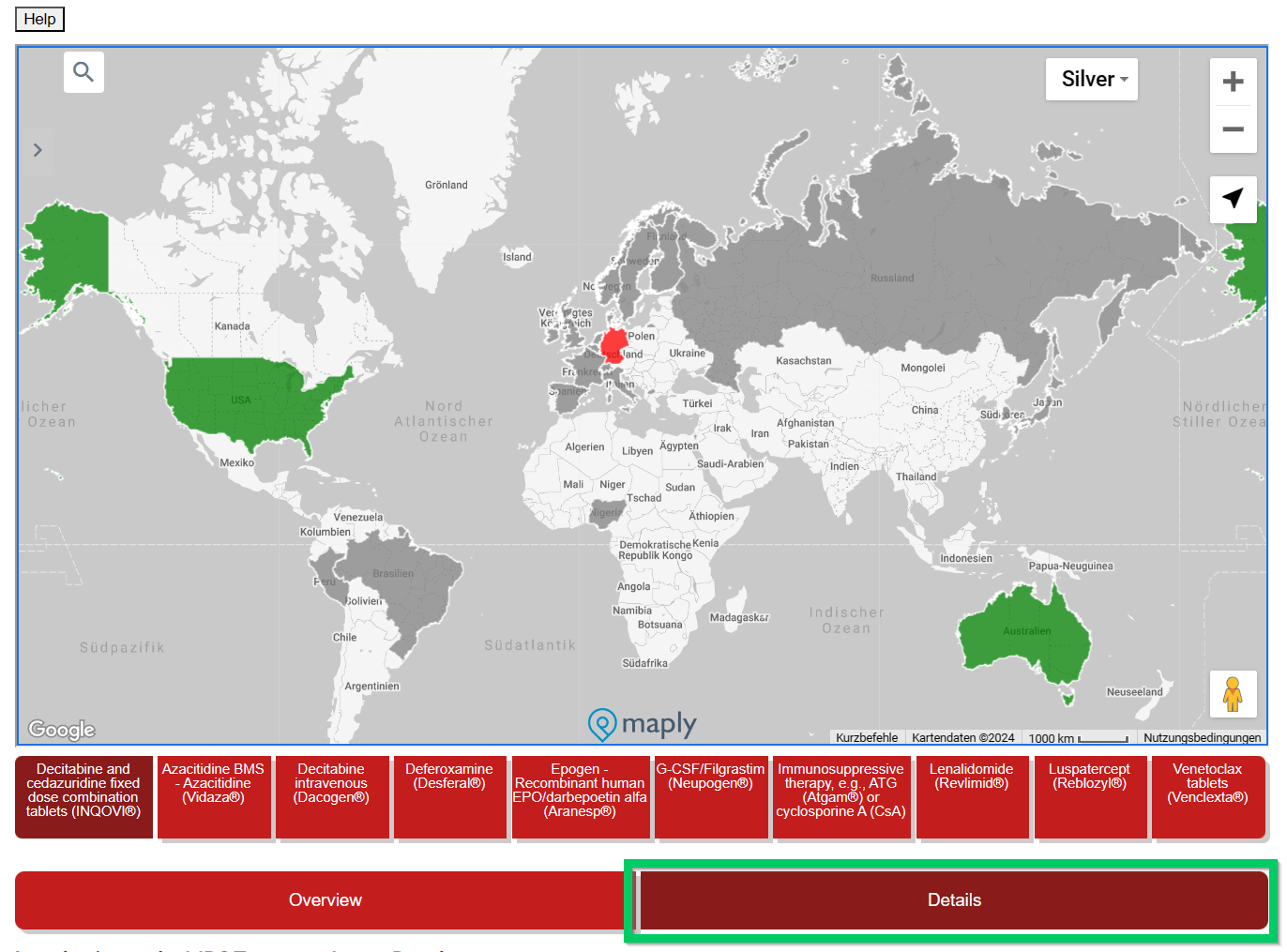
This overview is interactive and detailed information is displayed by moving the mouse. Under the country name there is a (pink) reference to the health insurance system (if known) in this country.



